
FOGRI carol service gets everyone in the Christmas sing
OVER 200 people packed out the magnificent Glasgow Cathedral on Friday December 12 to celebrate Christmas FOGRI style! Revd Mark Johnstone, Minister at the Cathedral,

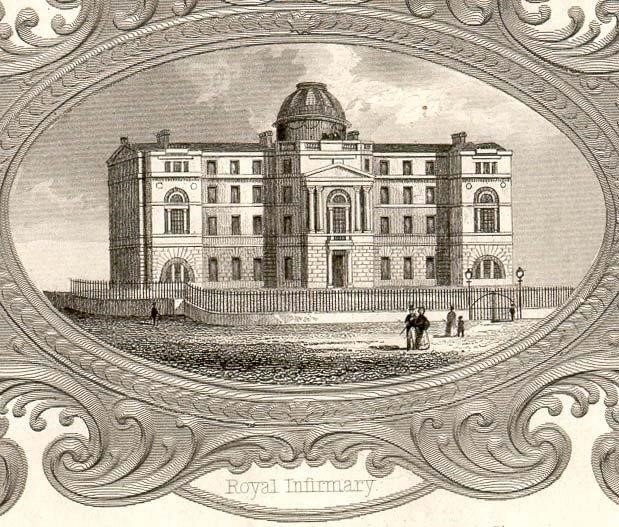
STEP inside a hospital which helped to change the world of medicine forever.
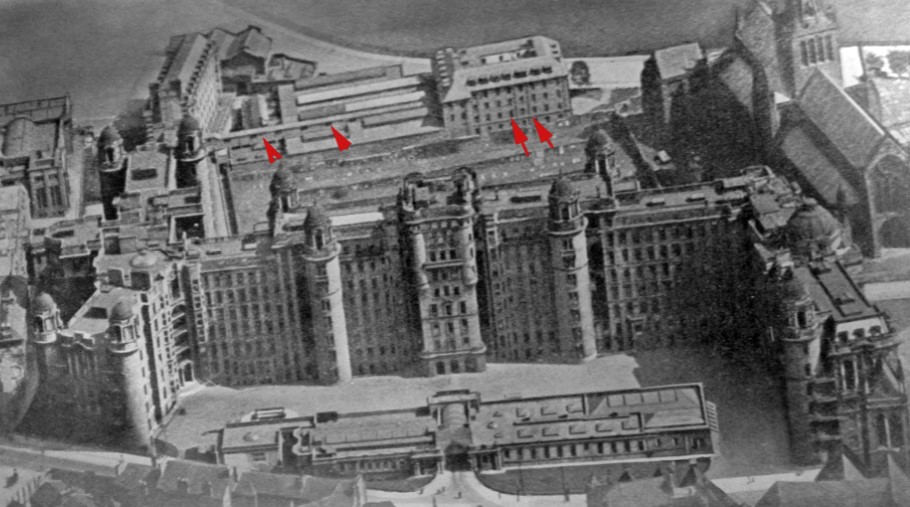
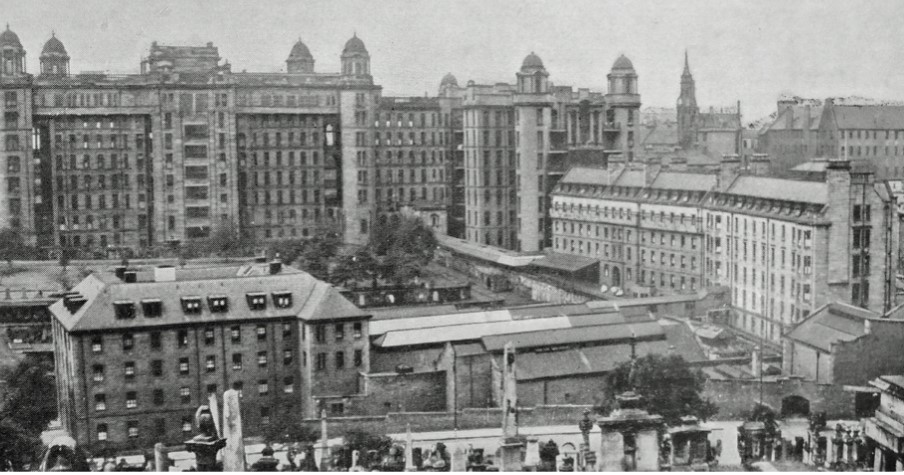
Glasgow Royal Infirmary’s first admission was way back in December 1794 – and since then it has been at the forefront of revolutionary advances.
This is the place where Joseph Lister discovered antisepsis, the location for the world’s first x-ray department and the venue where the first successful brain surgery took place. Rebecca Strong – who worked under the iconic Florence Nightingale – was the first matron here.
The Friends of GRI charity was established in May 2020 to celebrate this rich past. Two years later we opened a small museum, which the public can now enter free of charge on various days of the week.
We also have projects focusing on sustainability and enhancement of the workplace environment. A medicinal garden sits adjacent to the museum and bee hives are situated in a secret location on site. Our honey is sold each year and nearby restaurant Celentano’s includes GRI honey on the menu from head chef Dean Parker’s own GRI-based hive.
Our aim is to make GRI’s history accessible to the public via the museum and through hosting events commemorating the people and discoveries associated with the hospital.
If you would like to know more, have your own GRI memories to share, have come by any artefacts from the hospital or just want to be added to our mailing list then we’d love to hear from you at info@friendsofgri.org

OVER 200 people packed out the magnificent Glasgow Cathedral on Friday December 12 to celebrate Christmas FOGRI style! Revd Mark Johnstone, Minister at the Cathedral,

Christmas just wouldn’t be Christmas without our Carols at the Cathedral evening. Come along to Glasgow Cathedral for a right good dose of festive cheer

DONNA McCARTNEY admits focusing on her art has helped her through dialysis. Donna’s Sunshine On A Dull Day pastel drawing has formed the basis for

The concept of a medical museum was first floated more than a decade ago but life got in the way and the dream was never realised. In 2020, during the early part of the covid-19 pandemic, a charity was established. Under the auspices of the charity, dedicated social media accounts began to share some of the history of GRI. This generated interest, support and camaraderie during difficult and uncertain times. Virtual celebrations of Joseph Lister – #listerweek – and GRI women – #womensweek – followed and then an actual medical museum. The rest, as they say, is history!
The charity board comprises five trustees including our Chairman, Mr John Stuart. A wonderful team of volunteers staff the museum, maintain our garden areas, provide administrative support and run our website and media academy. We have no paid team members.














Mabel Mason was born on the 2nd of August 1876 in Cranston’s Waverley Temperance Hotel in Sauchiehall Street, Glasgow, opposite Copland and Lye, where Marks & Spencer is now. The hotel belonged to and was managed by her mother Mary Mason. Mary was married to George Mason, a pioneer in photography, who sold photographical materials in Buchanan Street.
Mary’s father, Robert Cranston, built and opened Cranston’s Old Waverley Hotel in 1848 in Princes Street in Edinburgh facing Walter Scott’s monument and on the opposite corner to Jenners. He was a remarkable man. He had a Waverley Hotel in Buchanan Street opposite the subway, and he also had a hotel in King Street Cheapside in London. The feature of all these hotels was that they were teetotal. No alcohol of any description was sold in them, and single ladies and families were safe and comfortable there. Robert Cranston was a Chartist and a passionate supporter of temperance, and this was approved of by many people. When Mary got married her father gave her the hotel in Sauchiehall Street as a wedding present and the hotel in Buchanan Street was sold. Mary Cranston became Mary Mason. She had three daughters and one son. The Cranston’s in Edinburgh flourished and had several high-class temperance hotels in London. Mary’s brother Robert became the Lord Provost of Edinburgh, and he had a large family.
Mary and her family moved out to Dowanhill in the West End of Glasgow which became popular for large families. Towards the end of the 19th Century Mary sent her two elder daughters, Elizabeth and Mabel to school in Paris for a year and then to Weimar in Germany which was a brilliant place at that time with shades of Goethe and Schiller watching the opera music and the arts. The result was that these two girls could speak French and German reasonably well. Mabel kept in touch with an Austrian girl at school with her in Weimar during both wars and took her daughter Elizabeth to Vienna to learn to sing in 1935. She was supposed to go for six months but stayed for four years under the watchful eye of Mabel’s friend Eda.
At the turn of the Century Mabel went to Julien’s studio in Paris and learned how to paint but was not able to get much painting done because she was about to be married. In 1902 Mabel married Charles Mackinlay, the youngest of a large Glasgow family. They were both interested in music, the arts, and the theatre.
Mabel joined the Royal Infirmary Dorcas Society in the early 1920s and she made a weekly visit to the Surgical Units on a Thursday with a pile of weekly magazines.
The Mackinlay family got its first motor car in 1925, a flat fronted Armstrong Siddeley, and Mabel learned to drive. She was an enthusiastic driver. She insisted that the car should have a flexible hood which could be opened because “these saloon cars are very stuffy!” She continued to drive well into her 80s and once a week and every week she would come up Cathedral Street in her open Austin 12 at 2.30 pm and the porters would stop the traffic to let her get in under the archway into the hospital. She never had a serious accident.
During the Second World War she took up her painting again and her great friend Dr Tom Honeyman, the Glasgow Art Director, encouraged her and organised two “one man” shows in a room in the McLellan Galleries. There would be about 40 pictures and they were sold like hot cakes, and they are scattered in houses all over Glasgow and its environs.
Quite early in the last war the Glasgow council asked people with accommodation available to take in a number of Polish refugees and Mabel said she would. A Polish girl of about 18 arrived at the front door and Mabel took her in. Her name was Maria. She had started a Science Degree in Poland and had fled to Paris with all her papers when the war began. She got to this country when France was overrun and was sent to Glasgow. Maria stayed for about 10 years during which time she went to Glasgow University and took an Honours Degree in Science, BSc (Hons) and went on to take a Doctorate PhD in Crystallography. She got a scholarship to go to Canada and she has been there ever since. She has now retired, married with two brilliant sons. She came to Europe frequently to lecture and always went to see Mabel – “her Scottish mother” – and take her out for dinner at the Malmaison or some other suitable restaurant! When Mabel died at the age of 94 and Maria retired, Maria instituted the “Mabel Mackinlay Prize” at the annual exhibition of the Royal Glasgow Institute of the Fine Arts. This Prize is awarded every year and at present is £1,000.
If it is a nice warm day and you would like to go for a stroll, why not go into the Necropolis and up to Quartus on your right-hand when you go through the gate. In the middle of the tombstones, you will see the iconic granite cross on a broad granite base (lairs 531 and 532) that Mabel commissioned when her husband Charlie died. Nearly all her family and their consorts are remembered there. She is content, she has her children round her and, she is near her Royal Infirmary.
Mabel had six children, four boys and two girls between 1904 to 1917. Willie was the eldest and had too busy a life to have time to get married. He was an accomplished pianist and singer, an outstanding and much sought for “after dinner speaker”, a director of companies, a member of the Royal Yacht Squadron and a good sailor and yachtsman and – most important – he was the Chairman of the Board of Management of the Glasgow Royal Infirmary after his friend Sir William Denholm. The rest of the family were spread out over India, London, Glasgow, Vienna, Hatfield, and South Africa.
Charlie, Mabel’s husband, died of cancer in 1934 at the age of 67. This was a great loss as they got on very well together. Most of the children had left home or were about to do so but Willie stayed with his mother most of his life. She was good company.
Thank you to Dr C J Mackinlay for providing this story.

To complete the payment for your sponsorship please click the button below to our SumUp payment link.
Once we have confirmed your payment we will email you to let you know your sponsorship purchase is complete!
Your message has been sent successfully. We will get back to you as soon as we can.
Born 23 August 1843 Rebecca Thorogood in Aldgate, London.
In 1865 she married Andrew Robert Strong, gave birth to Annie Ellen Strong same year and in 1866 she was widowed. The following year, Rebecca was accepted as a probationer at the Florence Nightingale Training School at St. Thomas’ Hospital and she became the first to complete training supervised by Miss Nightingale, with whom she remained in regular contact throughout the remainder of the great lady’s life. She initially worked in Winchester Hospital as Sister and in 1871, she was transferred to Netley Military Hospital
1874 she was appointed Matron at Dundee Royal Infirmary where Dr R. Sinclair was superintendent. With Sinclair’s support, she significantly improved standards of care and hygiene.
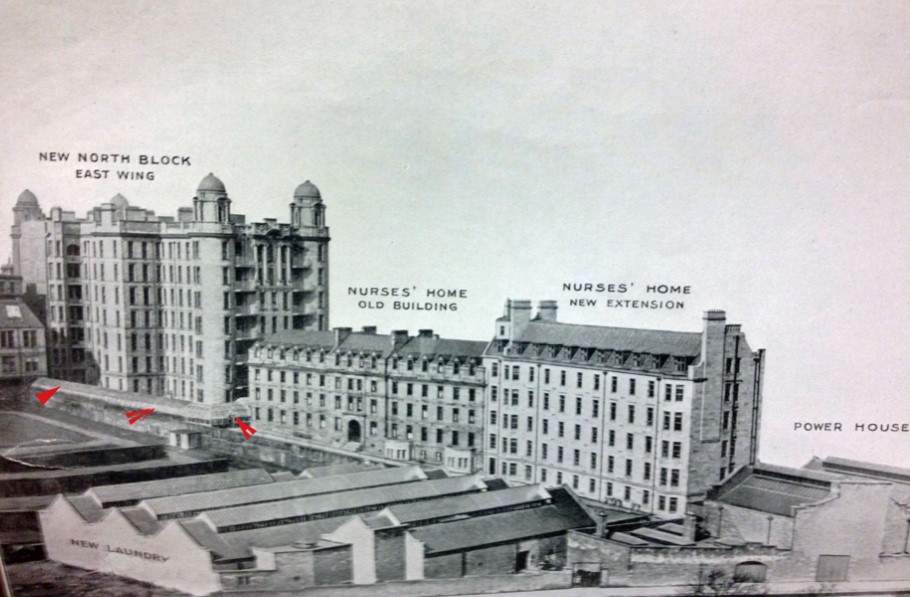
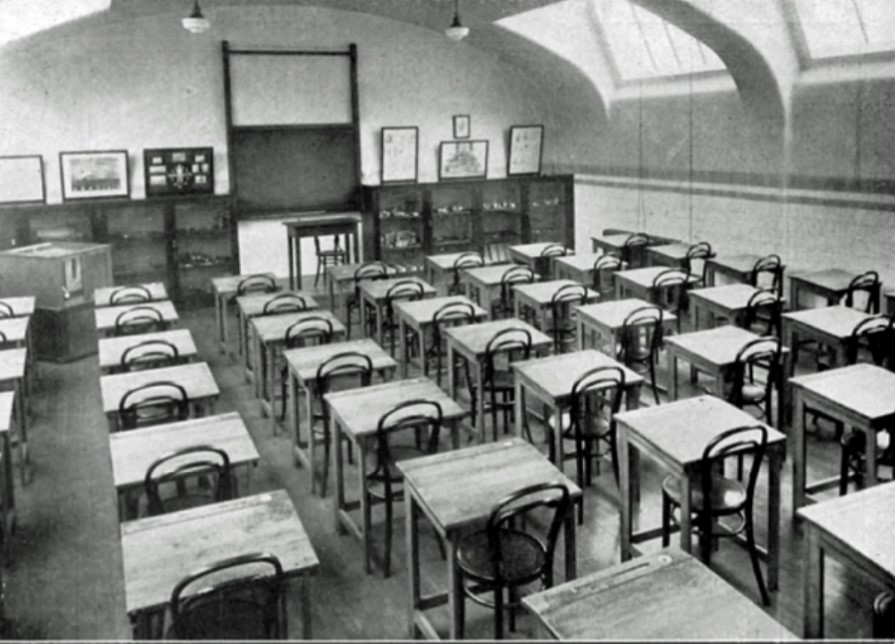
In 1879 she was appointed Matron at Glasgow Royal Infirmary and formed a professional alliance with the chief surgeon William MacEwen. With his support, she made improvements to hygiene and patient care, with specific attention to sterilisation techniques. She also applied her energies to better training for nurses with the ultimate aim of raising nursing to the status of a profession. Ultimately, Rebecca and MacEwen introduced the “Block Apprenticeship Programme” which was eventually adopted worldwide. Short periods of instruction for trainee nurses were followed by periods of practical experience on wards. Previously, nurses were expected to work up to 14 hours in hospital and then attend lectures in their own time. The pioneer Preliminary Training School was opened officially in January 1893 under an arrangement between GRI and St Mungo’s Medical College. The College had formerly been the GRI medical school and was eventually amalgamated with Glasgow University’s medical faculty in 1947.
In 1884, Rebecca Strong resigned her post, mainly in frustration at the unwillingness of the authorities to construct a nurses’ home.
She opened her own nursing home and accepted patients from MacEwen, with whom she remained in close contact.
In 1891 she returned to her post as Matron at GRI by which time a nurses’ home had been constructed. During the remainder of her working life at GRI she established the Scottish Nurses’ Association, with the objective of working towards a single system of state registration for nurses nationwide. This eventually happened in 1919.
1893 her Scheme of Nursing Education (Preliminary Training School) was introduced and became the foundation of all such schemes ever since. GRI became one of the foremost training centres for nurses in the UK. At the age of 64, in 1907, she retired from her post at GRI.
Following repeated petitions by friends and former colleagues, she was appointed OBE in 1938. In 1942, the MacEwen Medal in Surgical Nursing and the Mrs Strong Medal in Medical Nursing were established in GRI to commemorate the pioneering work of both individuals.
In 1943, she received congratulations from both the King and Queen on the occasion of her 100th birthday.
Rebecca Strong remained active almost right up to the time of her death. She travelled in Europe, the United States and Canada, discussing her experiences and tirelessly advocating equality of education for women. She firmly believed that intelligent women should not waste their lives, unproductive and unfulfilled. Her own intelligence, spirit and vision made an enduring difference to the nursing profession.
1944, April 24, in her 101st year, she was cremated in Chester, where she had gone to live with her great nephew, Dr Tindall and his wife, after being injured in a WW2 bombing raid on Glasgow.
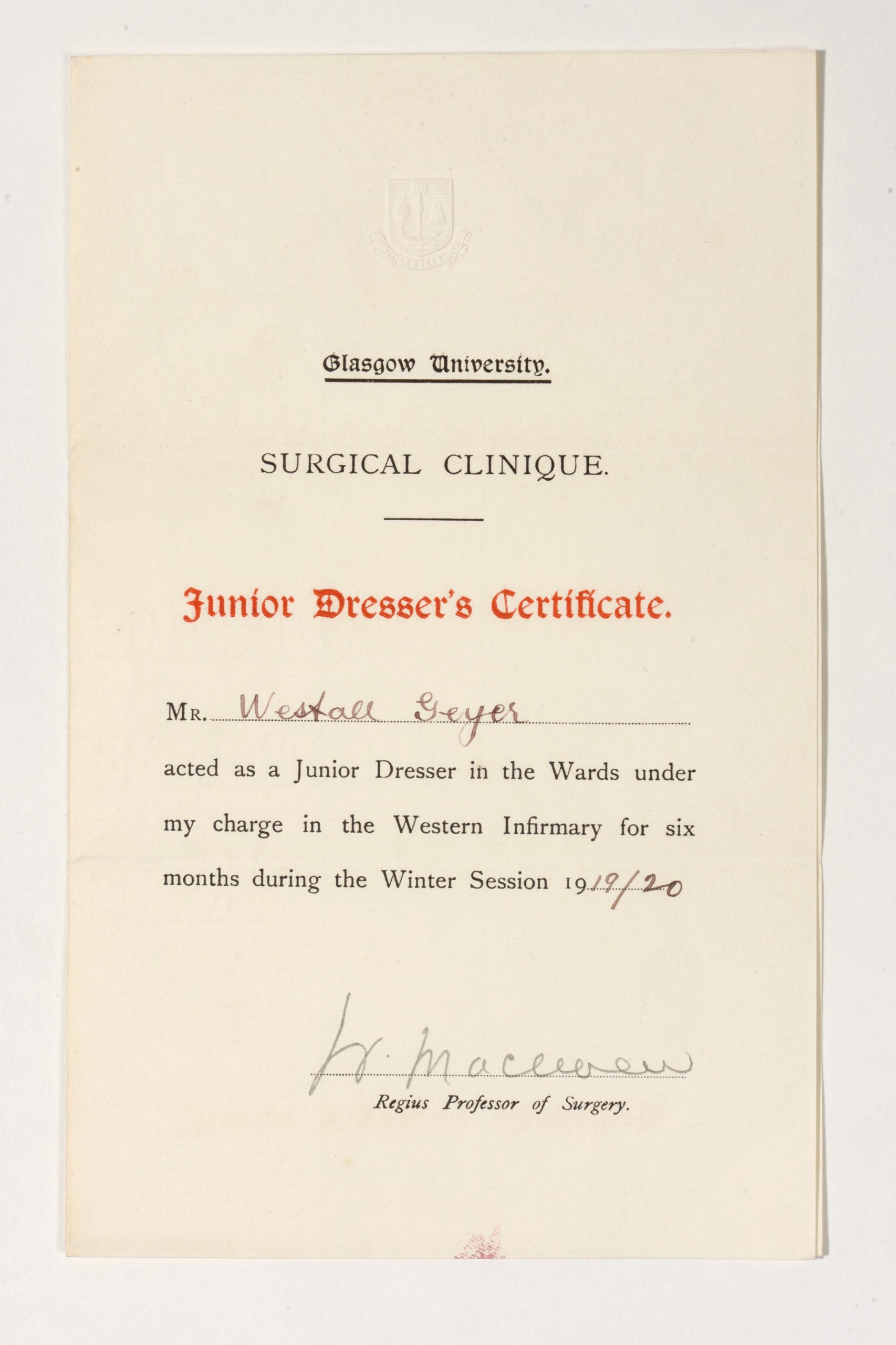
Rebecca Strong’s only child, Annie, moved to Scotland with her mother. In 1886 she married Adolph Hans Geyer in Govan. They had 5 children. Annie Ellen junior became a nurse; Adolph Robert and Westall Stelber both doctors. Westall’s son and Rebecca’s great grandson, David Geyer who is now 92 years old, remembers her fondly.

Rebecca Strong ‘“I am afraid I was rather a troublesome woman. As soon as one step was taken, I proposed another. This went on for a few years until it came to my asking for a home for nurses. This was too much and I was told quite plainly that I had gone too far and as I knew that the work could not advance without it, I resigned” Photograph courtesy of The Nightingale Museum
James Pringle was born in 1863 in Parramatta, Australia. His father, George Hogarth Pringle, was also a surgeon and studied under Joseph Lister during Lister’s time in Edinburgh, before emigrating to Australia. George Hogarth Pringle introduced Lister’s antisepsis practice to Australia.
In 1872, James returned to Scotland and was then educated at Sedbergh in North Yorkshire before entering Edinburgh University medical school, graduating in 1885. He then travelled in Europe and studied methods and techniques in Berlin, Hamburg and Vienna. Next, he underwent training in ophthalmology in Moorfields Hospital, London, before returning to Scotland, working first as House Surgeon in Edinburgh Royal Infirmary and then as House Surgeon at GRI under William Macewen. He became surgeon to GRI in 1896. With Macewen, he learned skills in brain surgery and was both innovative and successful in surgery for melanoma, tuberculosis and arterial sclerosis. His is most famous for the development of the Pringle Manoeuvre to minimise blood loss in hepatic surgery whilst surgeon at GRI.
Working at GRI, also afforded Pringle the opportunity to work alongside John Macintyre, who stablished the world’s first X-ray department in GRI in 1896. This, as well as his knowledge of Lister’s antisepsis practice (from both working in GRI and first hand from his father) allowed him to gain significant success and expertise in the management of fractures.
James Pringle, alongside William Macewen, was a staunch supporter of women in medicine. They were two of few senior figures who were very willing to have women students attend their clinics. Both Elsie Inglis and Louise McIlroy attended Dr Pringle’s clinics. Pringle was appointed Lecturer in Surgery and Anatomy Demonstrator at Queen Margaret College, in 1899. Queen Margaret College had, of course, been established for women students and taught women medical students from 1890/1891.
Pringle retired in 1923 and died at his home in Killearn, north of Glasgow, in 1941, aged 78.

Residents at the Old Royal Infirmary, Edinburgh, summer 1854: clockwise from left, John Beddoe (seated left), John Kirk (back row), George Hogarth Pringle (James H Pringle’s father, back row), Patrick Heron Watson (back row), Alexander Struthers (seated right), David Christison (seated in front, right), Joseph Lister (seated in front, left). Image Wellcome Collection Attribution 4.0 International (CC by 4.0)
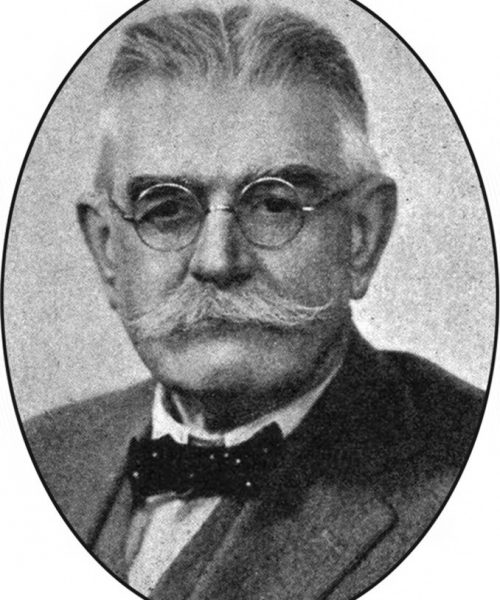
James Hogarth Pringle
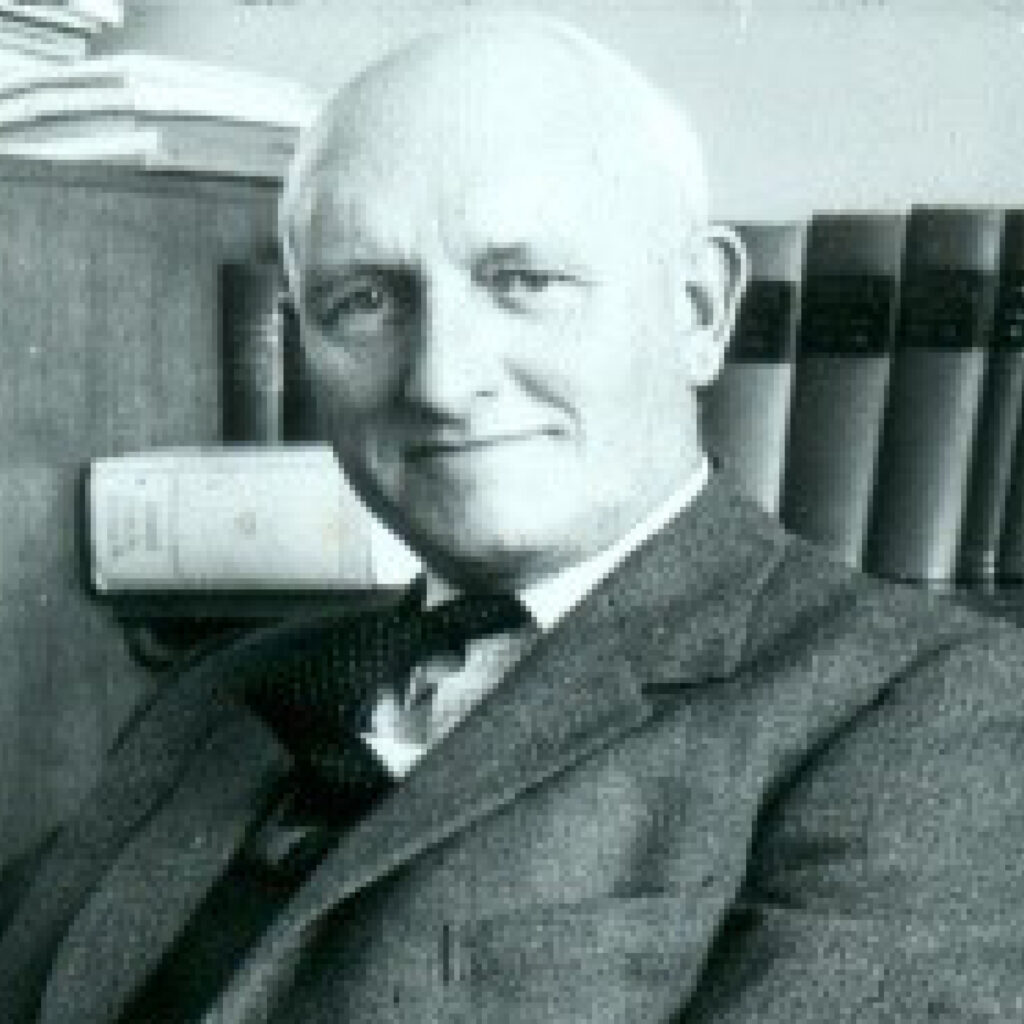
John Martin Munro Kerr MD, L.L.D Glasg, F.R.F.P.S.,F.R.C.O.G. 1868-1960
Known as Munro Kerr, he had a glittering career which began with an education at Glasgow Academy and then Glasgow University from where he graduated MBChB in 1890 and MD in 1909.
Munro-Kerr chose to specialise in Obstetrics and Gynaecology and spent several post-graduate years studying in Dublin, Jena and Berlin before, in 1894 becoming assistant to The Regius Professor of Midwifery, Murdoch Cameron and then in 1900 taking up the post of visiting surgeon to the Glasgow Royal Maternity Hospital or ‘Rottenrow’.
In 1907, he took up an appointment as a gynaecological surgeon at the Western Infirmary in 1900 and in 1911, Munro Kerr became the first occupant of the Muirhead Chair of Midwifery and Gynaecology at Anderson Medical College, Glasgow. In 1927, he was appointed as Regius Professor of Midwifery at Glasgow University and held this post until his retirement in 1934. On his retirement from the teaching staff and after forty years’ service, the University conferred on him the honorary degree of L.L.D. He was a leading authority in his specialty and authored several books include Operative Obstetrics (1908), The Combined Textbook of Obstetrics and Gynaecology (1923) and Maternal Mortality and Morbidity (1933). He was awarded the Katherine Bishop Harman prize for his monograph on Maternal Mortality and Morbidity.
Munro Kerr chose his specialty at a time when childbirth was hazardous, particularly for women from deprived areas where malnutrition and insanitary living conditions increased the risk of infection and of death. He witnessed some of the first caesarean operations performed in Scotland (Murdoch Cameron performed the first at Rottenrow on 10th April 1888) and directed his efforts towards improving the safety of the operation. In the early 1920s only a few younger surgeons in Glasgow and Edinburgh were conducting the operation and by the 1930s it was still rarely performed in England. It was not until after WW2, in 1949, that the caesarean section was finally accepted, universally, as a safe and essential procedure to ensure the lives of many mothers and their babies.
At the first post-war obstetrical congress, after several speakers had provided evidence that the caesarean section was indeed safe, Munro Kerr was unexpectedly called to address the conference. He threw up his arms and loudly cried “Hallelujah! The battle’s o’er; the victory’s won!”
Munro Kerr was one of the founders of the Royal College of Obstetrics and Gynaecology and and was its first vice president between 1929 and 1932. In 1948 when the college was granted a royal charter, honorary fellowship was conferred upon him. From 1933 to 1936, Munro Kerr served as president of the Royal Faculty of Physicians and Surgeons in Glasgow. In 1950 he was the first recipient of the Royal Society of Medicine’s Blair-Bell medal.
Following his retirement, he moved to Canterbury and during WW2 he acted as medical superintendent to the Kent and Canterbury Hospital. Well into old age he continued to contribute to medical journals and he also wrote reminiscences and medical sketches. In 1956 he travelled back to Glasgow to deliver the first William Hunter memorial lecture at the Royal Faculty of Physicians and Surgeons.
Munro Kerr was a keen golfer an held the position of Captain of Glasgow Golf Club in 1922
Friends and colleagues described Munro Kerr as a natural leader blessed with a great personality and a sense of humour and a unique ability to inspire those around him.

Courtesy of Douglas Mack
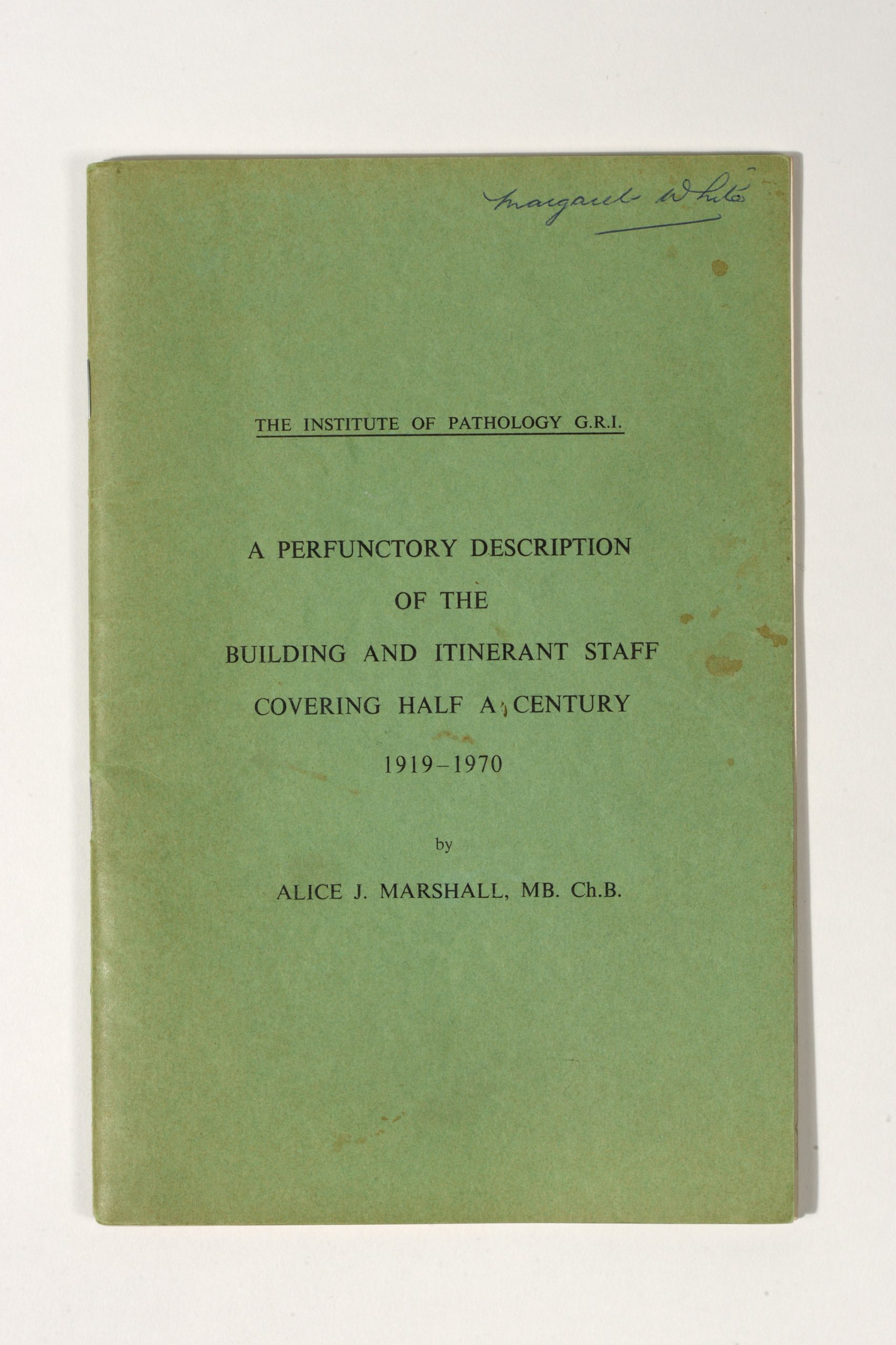
Alice Julia Marshall was born in Stirling on 12th April, 1891. She matriculated at Glasgow University in 1912 and graduated MB ChB in 1917. She became a resident at GRI and joined the Pathology department on graduating.
Dr Marshall specialised in Gynaecological Pathology. She edited Professor John H. Teacher’s textbook on the subject after his death and also co-authored several papers on the pathology of the heart.
Along with Professor J.A.G Burton, she provided a blood transfusion service for the GRI, prior to centralisation of blood transfusion services under the NHS.
She retired in 1956 at the age of 64 but continued to work with Professor Burton cataloguing pathological specimens of historical importance: the catalogue of Pathological Preparations of Dr. W. Hunter, Sir William Macewen, Professor J.H. Teacher and Professor J.A.G. Burton were published in 1962. Two further publications followed – the Pathological Preparations of Dr. W. Hunter in the Museum of Anatomy Department and Anatomical preparations of Professor John Cleland (1970).
Although recently retired, she also participated in the 1957 mass radiography campaign, during which 714,915 Glasgow citizens were x-rayed in an effort to eradicate pulmonary tuberculosis.
Dr. Marshall also continued to play a role in the training of junior pathologists well into later life.
She was one of the earliest females to become a Member of the Royal Medico Chirurgical Society of Glasgow.*
Dr. Marshall did not marry but was believed to have a close personal relationship with Professor Burton. She died in 1987.
*Records of the society are held by RCPS Glasgow
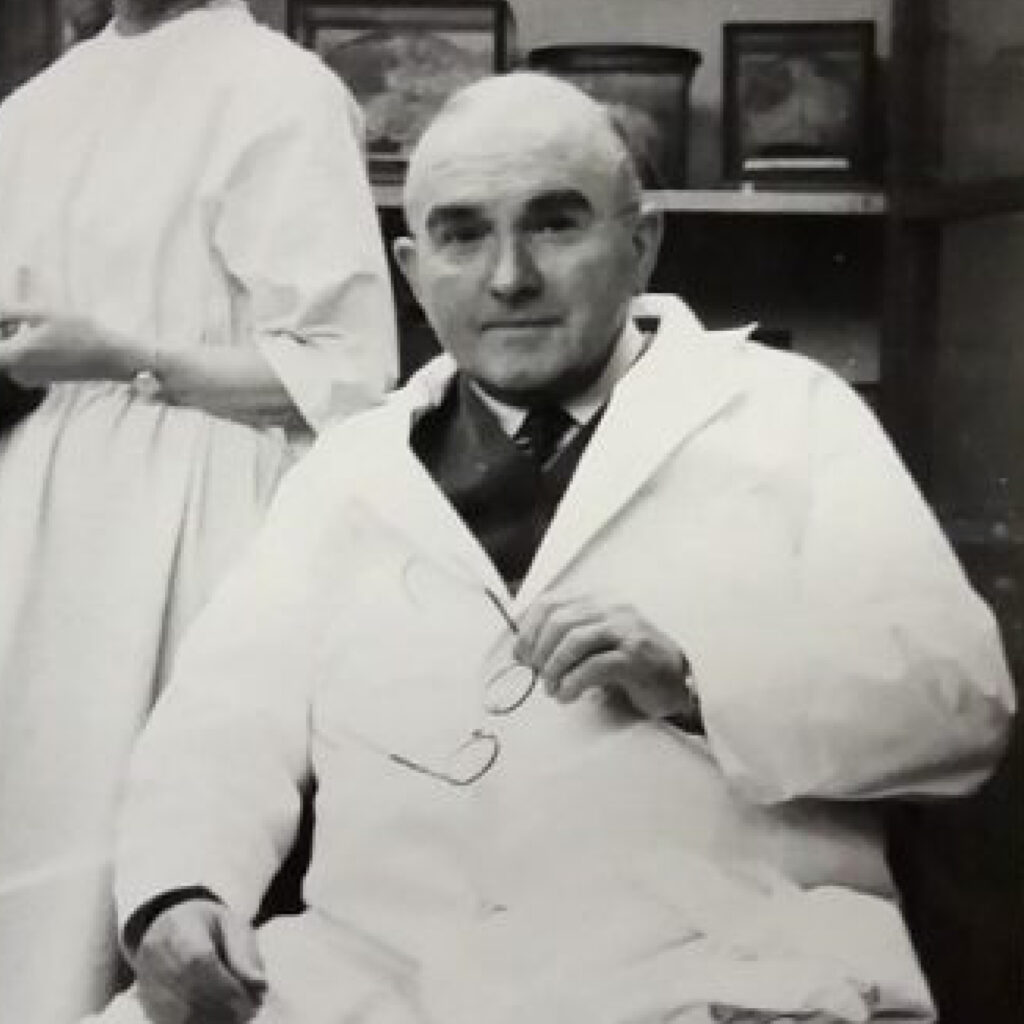
Dr Alice Marshall with Professor John Burton
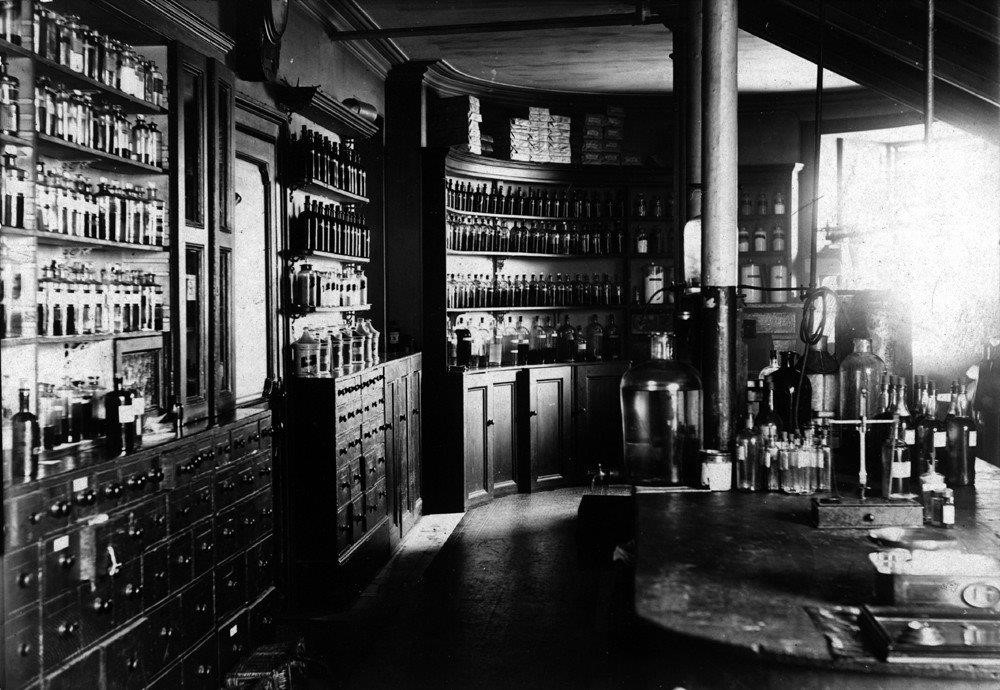
John Macintyre (1857-1928) established the first radiology unit in the world at GRI, establishing in 1902 a unit built specifically for the purpose. The x-rays he was able to produce of numerous parts of the body, were of significant help to doctors and surgeons in diagnosis and treatment.
Macintyre had begun life training as an electrician, but switched to medicine and graduated MB, CB from Glasgow University in 1882. He worked as a ship’s surgeon in London and in Europe before returning to Glasgow as Surgeon for Diseases of the Throat at Anderson’s College Dispensary. At this time he also established a private practice treating actors and singers, which became quite lucrative.
In 1885, spurred by his early knowledge of electricity and a conviction that electricity had potential uses in medicine, he became Consulting Medical Electrician to GRI. in 1887 he set up a department for the use of electricity in medicine and it was from this that he developed, with the assistance of Archibald Fauld and an engineer called William Bottomley, the first radiology unit in the world.
He was awarded an LLD in 1920. Watch this short video about Macintyre and X rays at GRI here
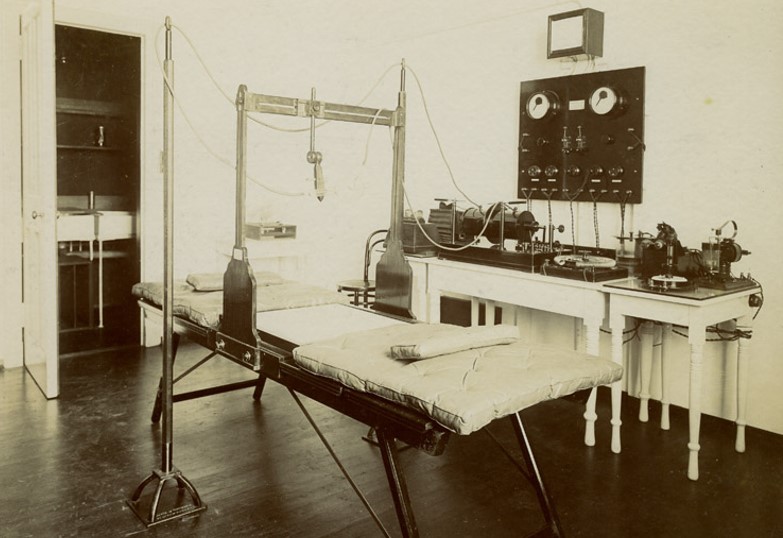
The first X-ray department in the world was located at GRI. Photograph courtesy of NHSGGC Medical Illustration Services
Baron Joseph Lister (1827-1912) was a pioneer of antiseptic surgery. He was Professor of Surgery at Glasgow University 1860-69 and, during this time he introduced the use of carbolic acid to disinfect surgical instruments in cases of compound fracture. He became a peer in 1883 and Lister House halls of residence (now demolished) were named after him.
Lister was born in London and studied medicine at University College London. He became a Fellow of the Royal College of Surgeons and moved to Edinburgh to study under James Syme, a renowned surgeon. He married Syme’s eldest daughter, Agnes, and at the age of 33 he was appointed Regius Professor of Surgery at Glasgow University. It was after this that he read the papers of Louis Pasteur, the French biologist and micro biologist. Lister began applying carbolic compounds as an antiseptic to surgical wounds. Although the results were positive, he received much scepticism and outright opposition from some of his colleagues. His methods were adopted in Germany, USA and France before Great Britain at last followed suit. In 1877 he returned to London at the age of 50 to become Professor of Clinical Surgery at King’s College.
Sir William Macewen (1848-1924, knighted in 1902) graduated with a medical degree from Glasgow University in 1872. He was greatly influenced by the work of Joseph Lister. He became assistant surgeon at GRI in 1874 and was promoted to full surgeon in 1877, Macewen is widely considered to be the father of brain surgery, having further developed Lister’s work in sterilisation, disinfection and antisepsis. Macewen carried out the world’s first successful brain surgery in 1879, removing a tumour (a left frontal meningioma) from a young woman. She lived for a further eight years. He made significant contributions also in orthopaedics, the removal of infected lungs in the treatment of tuberculosis and lung cancer and endotracheal anaesthesia, the method for which he described in 1880 and which is still in use today.
Macewen also believed in the advancement of training and conditions for nursing and nurses as an essential support to developments in surgery and medicine, and in 1880 he began a training programme for nurses, with a focus on sterilisation, under the management of Mrs Rebecca Strong, Matron of GRI. The two formed a formidable and effective partnership and eventually their training methods for nurses were adopted worldwide. In 1942, the Macewen Medal in Surgical Nursing and the Mrs Strong Medal in Medical Nursing were established at GRI to commemorate the work of both individuals.
In 1883, Macewen was appointed Surgeon to the Royal Hospital for Sick Children in Glasgow and in 1892 he became Regius Professor of Surgery at Glasgow University, a post which Lister had held when Macewen was a student. At this time he also moved his surgical activities to the Western Infirmary, Glasgow.
Macewen continued to innovate well into his later years, He became the first surgeon appointed to the Princess Louise Hospital for Limbless Soldiers and Sailors (now Erskine Hospital) and with the help of engineers from Yarrow’s shipyard on Clydeside designed artificial limbs for patients of the hospital.

William Macewen (standing to left, hand on patient) operates as Rebecca Strong looks on (right wearing grey dress and black cardigan). Photograph courtesy of NHSGGC Medical Illustration Services
Baron Joseph Lister (1827-1912) was a pioneer of antiseptic surgery. He was Professor of Surgery at Glasgow University 1860-69 and, during this time he introduced the use of carbolic acid to disinfect surgical instruments in cases of compound fracture. He became a peer in 1883 and Lister House halls of residence (now demolished) were named after him.
Lister was born in London and studied medicine at University College London. He became a Fellow of the Royal College of Surgeons and moved to Edinburgh to study under James Syme, a renowned surgeon. He married Syme’s eldest daughter, Agnes, and at the age of 33 he was appointed Regius Professor of Surgery at Glasgow University. It was after this that he read the papers of Louis Pasteur, the French biologist and micro biologist. Lister began applying carbolic compounds as an antiseptic to surgical wounds. Although the results were positive, he received much scepticism and outright opposition from some of his colleagues. His methods were adopted in Germany, USA and France before Great Britain at last followed suit. In 1877 he returned to London at the age of 50 to become Professor of Clinical Surgery at King’s College.
He has been described as “the father of modern Surgery” and “the greatest surgical benefactor to mankind”. Queen Victoria made him a baronet in1883 and he was given a full peerage in 1897, designated Lord Lister of Lyme Regis.Learn more by watching our Lister week webinars HERE
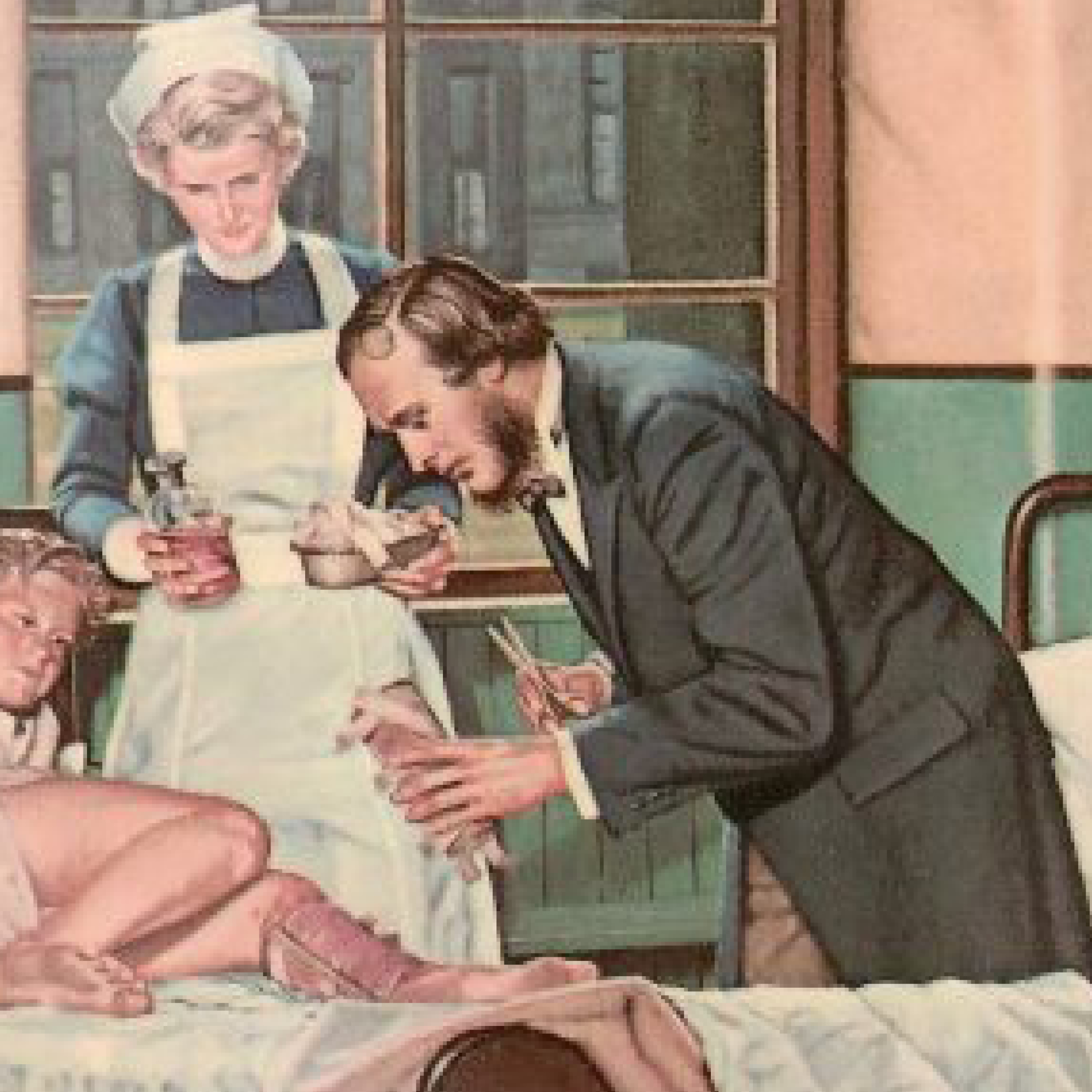
Joseph Lister treats James Greenless
Professor George Jardine (1742-1827) was a leading light on the committee of subscribers which had promoted the construction of GRI. It is fitting, therefore that he was the first manager of GRI having been appointed secretary in 1792, prior to the official opening in 1794. He was born in Wandal in Lanarkshire and matriculated at Glasgow University in 1760, graduating MA in 1765. At the time of his appointment as manager of GRI, Professor Jardine was Professor of Logic and Rhetoric at the University of Glasgow; a post he held between 1774-1827. Additionally he was Clerk of the Senate 1881-82. He is buried in the Lindsay plot (his wife’s family) in the Glasgow Cathedral cemetery.

Professor George Jardine
David Paton Cuthbertson (9/5/1900 – 15/4/1989) was born in Kilmarnock and was educated in Kilmarnock Academy. After a spell in the Royal Scots Fusiliers, he went to Glasgow University where he graduated first in Chemistry and then in Medicine. At the age of 26, he was invited to take up a post at Glasgow University, being both the first lecturer In Pathological Biochemistry and the first biochemist based at Glasgow Royal Infirmary.
In his first few weeks a surgeon asked him why fractures of the tibia were slow to heal. The search for the answer to this question ultimately defined his lifetime’s career. By measuring basic chemical constituents – nitrogen, phosphorus, sulphate and calcium – in urine, blood, faeces, tissue and food, and subsequently Basal Metabolic Rate to understand energy expenditure, he developed a basic understanding of how the body’s metabolism responds not only to injury such as broken bones but also to infections and inflammation. He described an early “ebb phase of depressed vitality” when the oxygen utilisation and body temperature decreases. This was followed by what he described as a “flow phase” with increases in metabolic activity, muscle breakdown, temperature, and oxygen utilisation. He recognised that this mobilisation of protein from muscle provided amino acids which would lead to repair and renewal of tissue.
It was clear to Cuthbertson that good nutrition played an important role in recovery of critically traumatised patients and so his interest expanded into this scientific field. Two of his early papers provided the foundation for modern nutritional therapy of seriously ill or injured patients, by attempting to limit loss of body components in early periods and ensuring an adequate supply of nutrients to act as substrates during the recovery phase
In 1934, he was invited to take up the Grieve lectureship in physiological biochemistry at Glasgow University from 1934-1945, since it offered him access to a wider range of academic colleagues and physiological techniques.
In the late 1930s, Cuthbertson became interested in patients with severe burns since these patients have a large metabolic response to their injury. He applied to the Medical Research Council for a grant to employ a junior colleague to further research his ideas for improved treatment. Because of the importance of improving the treatment of burns in the on-going Second World War, he was offered sufficient funding to establish a team of senior researchers which resulted in a novel therapy – intriguingly named MRC Cream Number 9 – which was successfully employed for the remainder of the war. With the rapid success of this project, Cuthbertson was seconded to the MRC and also to act as an advisor on optimal nutrition in the armed forces.
Sir David Paton Cuthbertson

Case notes from a patient with a broken tibia and fibula.
In 1945 when Lord John Boyd-Orr – famed for overseeing Britain’s food policy during World War II – retired from the directorship of the Rowett Institute, which was established in Aberdeen as the UK’s centre of excellence in nutritional research, Cuthbertson was the obvious choice as successor. Under Cuthbertson’s stewardship the institute expanded enormously. At the time there was perceived to be a post-war threat to food supply because of a potential Russian blockade of supplies and so Cuthbertson’s initial remit was to research animal nutrition with the goal of expanding Britain’s capacity for home food production.
Under his direction, the institute created a farm, and facilities for research in protein and carbohydrate chemistry, microbiology, enzymology, applied biochemistry, physiology, pathology, animal behaviour, applied animal nutrition and statistics. In its jubilee year in 1963, the number of staff had increased fourfold. Aberdeen was not perhaps the most alluring location to attract scientists, but Cuthbertson’s powers of persuasion and his reputation were such that he could still engage the best. One was Dr Richard Synge who in 1952 was awarded the Nobel Prize for Chemistry.
One early report which demonstrated the breadth of his nutritional understanding and gave him much satisfaction was his survey of ‘Nutrition in Newfoundland’ in 1947 with many important public health recommendations.
During his twenty years at the Rowett Institute, his personal reputation and that of the Institute came to be recognised internationally and his involvement in research of animal and human nutrition was set on the world stage. As well as being president of the UK’s Nutrition Society and the British Society of Animal Production he was also president of the International Union of Nutritional Sciences.
He was awarded CBE in 1957 and on his retirement in 1965 he was knighted. He then began the third phase of his career, returning to the Department of Clinical Biochemistry at Glasgow Royal Infirmary to continue his metabolic research. He developed an interest on the effect of elevated environmental temperature in reducing the metabolic response, and had special investigative rooms built to study this.
He was a regular contributor at international meetings and also acted as mentor to other younger scientists and academic clinicians. In 1979 the European Society for Parenteral and Enteral Nutrition was founded to act as a major international forum for the understanding of nutrition in disease, with an emphasis towards artificial nutrition. He was delighted when this new Society chose to name one of the two Plenary lectures after him, this being one of the most prestigious lectures still given annually in the field of Clinical Nutrition. The Society is now known as ESPEN, the European Society for Clinical Nutrition and Metabolism.
Sir David was clearly very bright but other facets of his character were just as important to his success. He was enormously energetic both at work and play. Much of his early research was carried out in the evenings and weekends when he would carry out much of the analytical work himself. Despite his considerable workload he never relaxed from opportunities to expand his research into other areas. When he ‘retired’ at the age of 65, Glasgow Royal Infirmary was only too happy to create an honorary position which enabled him to work right up till his death at the age of 89.
He was an enthusiastic golfer from an early age, his father also being a keen golfer. He was also a skilled painter of water colours which he showed at a number of exhibitions.
Although Cuthbertson could be occasionally be inattentive to administrative matters – for example he forgot to give notice that he was retiring from MRC – when it came to research, his attention to detail was absolute. In his twenties he realised that he could not rely on busy nurses to collect samples and record data and so he convinced medical staff that a separate metabolic ward with a kitchen for preparing tailored meals should be established so that data from his research patients would be meticulously collected. To exclude the possibility that confinement to bed might cause the metabolic changes seen in injured patients, he recruited a control group of students (at a rate of £2 per week) to lie in bed with a leg in splints for up to 2 weeks.
One of Cuthbertson’s greatest contributions to science came from his desire to educate. During his career he regularly contributed at international nutrition conferences, he wrote 5 books and published over 400 scientific papers and reviews and updates on the progression of knowledge regarding the metabolic response to trauma, infection and critical illness.
Perhaps the most important aspect of his success was his personal nature. He was a gentle gentleman – helpful, affable, engaging and enthusiastic – qualities which enabled him to engage positively with all his associates. He acted as a role model and inspiration to many.
Beatrice Clugston was born in September 1827, the eldest of five children in a village near the East End of Glasgow to a prosperous, hard-working devout Christian family. Her father had a factory making power looms and also a bleaching works in Avonbank Larkhall. He and his family were responsible for the well-being of his many workers and their families. Beatrice was introduced to these responsibilities at an early age. She and her mother visited homes when family members were ill taking food or money as needed. Her early years must have known great sadness because three of her siblings died before they were 10 years old.The family moved into Glasgow and Beatrice started a remarkable life of service to the city. She worked among the poor, among alcoholics and prostitutes and visited women prisoners in a Glasgow jail.

Beatrice Clugston
Hector Clare Cameron was born in Guyana, where his father was a sugar planter, on 30 September, 1843.
He came to Scotland to study at St Andrews, Edinburgh and finally attended Glasgow University, graduating MB CM in 1866, MD in 1868. He studied then trained as a surgeon under Joseph Lister. Cameron was a devotee of Lister’s antisepsis techniques and promoted the practice widely. In 1873 he became visiting surgeon at GRI. In 1881 he moved to the Western Infirmary, as senior visiting surgeon. Cameron was Professor of Clinical Surgery at Glasgow University 1900-1910. He was also President of the Faculty of Physicians and Surgeons of Glasgow 1897-1900.
Knighted by Queen Victoria in 1900, awarded an honorary LLD in 1912, he was then awarded CBE 1918 by King George V.
In 1927 he published REMINISCENCES OF LISTER, AND OF HIS WORK IN THE WARDS OF GLASGOW ROYAL INFIRMARY.
He died in 1928 and is buried with his family at the south end, east side upper plateau of the Glasgow Necropolis.

Sir Hector Clare Cameron as a young man. Image Wellcome Collection License Attribution 4.0 International (CC BY 4.0)

Sir Hector Clare Cameron, photographed by T Annan & sons. Image Wellcome Collection Attribution 4.0 International (CC BY 4.0)